Opinion Article - (2022) Volume 11, Issue 4
CLINICAL IMPORTANCE OF GERIATRIC DISORDERS DURING ACUTE HOSPITALIZATION
Barros Siggins*Received: Nov 28, 2022, Manuscript No. JHRP-22-84137 ; Editor assigned: Dec 02, 2022, Pre QC No. JHRP-22-84137 (PQ); Reviewed: Dec 16, 2022, QC No. JHRP-22-84137 ; Revised: Dec 23, 2022, Manuscript No. JHRP-22-84137 (R); Published: Dec 30, 2022, DOI: 10.30876/2321-0958.22.11.193
Description
A complicated group of clinical signs and symptoms in older persons known as Geriatric Conditions (GCs) do not fall neatly into one specific illness category. A common GC in the aged population is dizziness, which can be brought on by a number of pathogenic and aging-related functional impairments. However, just like in the younger population, dizziness is frequently linked to a particular pathology, like an inner ear disorder. GCs are multifactorial and happen when older persons become more susceptible to situational difficulties as a result of the cumulative impacts of numerous systems being impaired. Despite the fact that its components have not been precisely described, the idea of GCs, also known as geriatric syndrome, has gained widespread acceptance.
Numerous studies have examined the clinical implications of GCs and shown that they increase the risk of hospital admission and mortality in elderly people who live in the community. Additionally, several studies have discovered a link between GCs and readmission following an acute hospitalisation. In contrast to older adults who live in the community, the clinical importance of GCs in the acute care context has not received as much research.
Hospital-Acquired Complications (HACs), which are a barrier to safe and efficient treatment and should be avoided as much as possible, are frequently associated with hospital admission in older persons. Delirium, falls, functional decline, decubitus, and incontinence are examples of HACs that can be classified as GCs if they start occurring after a hospital stay. The correlation between GC at admission and the occurrence of HACs while hospitalised is still poorly understood. Furthermore, little is known regarding the relationship between GCs and frailty and polypharmacy, two conditions that are known to increase the risk of unfavourable outcomes in a variety of circumstances and are generating more and more interest in the geriatric area.
In this study, we sought to shed light on the clinical significance of GCs in acute care, first by examining the cross-sectional relationship between GCs and frailty/polypharmacy at the time of admission to an acute care geriatric ward and then by prospectively examining the relationship between GCs and the incidence of HACs and their effects after discharge.
We discovered a substantial correlation between GCs and the degree of fragility at admission. Age-related reductions in physiological reserve lead to fragility. A link between frailty and GCs seems plausible given that GCs are also age-related. Additionally, we discovered that this link was unrelated to any multimorbidity that the CCI score may have captured, suggesting that GCs have a different clinical meaning than discrete disorders. We were able to identify this correlation and validate a cause-and- effect relationship between frailty and GCs thanks to the cross- sectional design element. A build-up of age-related GC symptoms may contribute to the development of frailty, or the symptoms of GCs themselves may constitute a phenotypic of frailty brought on by a reduction in physiological reserve with age.
In addition, there was a connection between GCs and the amount of drugs recommended at admission, which was unrelated to multimorbidity. This research shows that medical professionals should look out for GC symptoms rather than just treating specific illnesses in the elderly. Although symptom relief is crucial for the senior population, drugs recommended to do so frequently continue to be taken even after they are no longer required. While the use of many drugs to treat GC symptoms leads to polypharmacy, there may be a two-way relationship between GCs and polypharmacy. Numerous regularly prescribed drugs may cause or worsen GC symptoms, leading to a rise in the number of drugs administered.

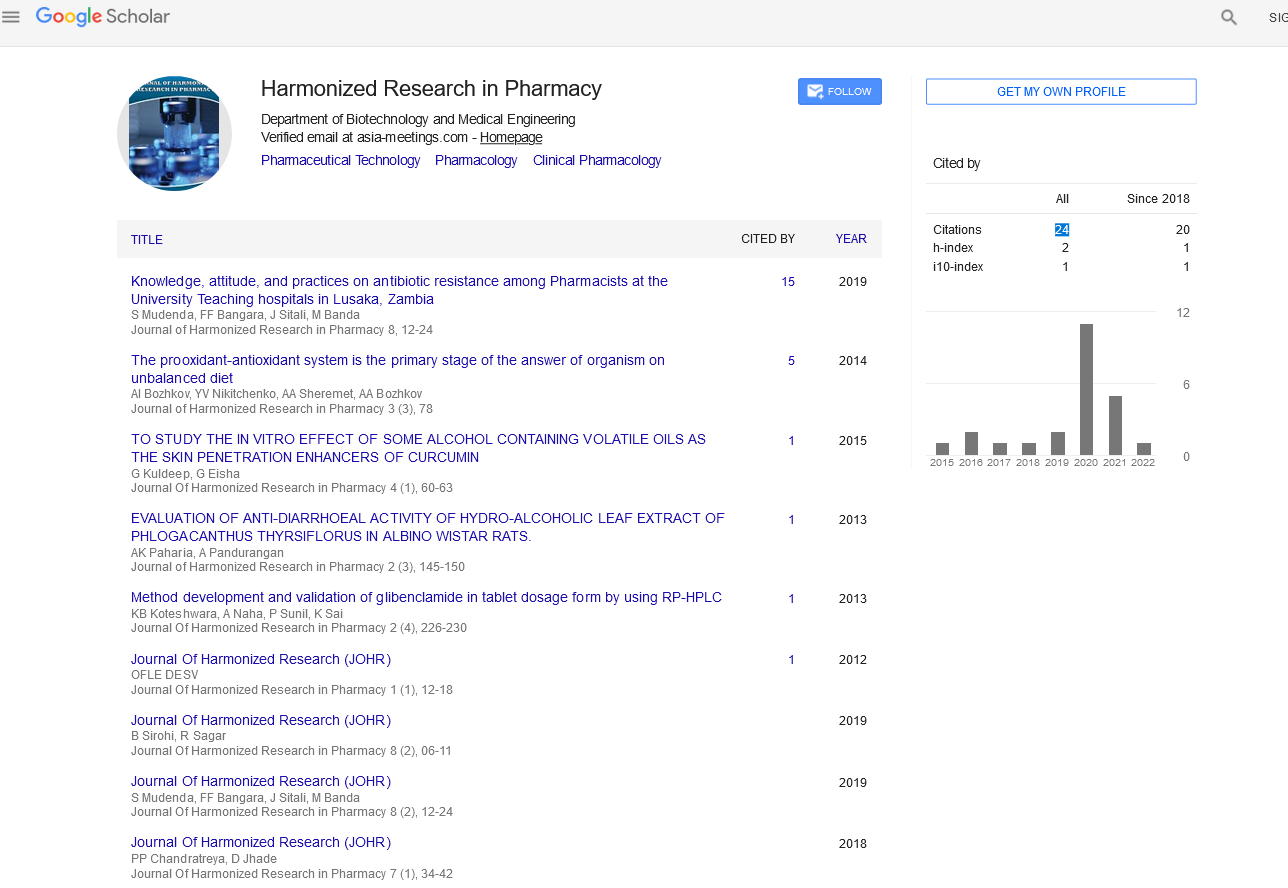
Google Scholar citation report
Citations : 147
Journal of Harmonized Research in Pharmacy received 147 citations as per google scholar report