Commentary - (2022) Volume 11, Issue 2
CLINICAL PHARMACISTS CONTRIBUTION TO THE DEVELOPMENT OF CLINICAL PHARMACY
Raniel Kamran*Received: May 27, 2022, Manuscript No. JHRP-22-69465 ; Editor assigned: May 30, 2022, Pre QC No. JHRP-22-69465 (PQ); Reviewed: Jun 13, 2022, QC No. JHRP-22-69465 ; Revised: Jun 20, 2022, Manuscript No. JHRP-22-69465 (R); Published: Jun 30, 2022, DOI: 10.30876/2321-0958.22.11.181
Description
Clinical pharmacists are in a perfect position to influence hospital doctors’ prescription since they have the necessary therapeutic knowledge and frequently interact with prescribers. To impact prescription, hospitals have used two basic tactics. These include the creation of hospital regulations governing the prescription process and the post-graduate training of individual pharmacists to advance their therapeutic skills and clinical process expertise.
The majority of hospitals have a hospital formulary and a statement of prescribing policy that permits the use of approved names rather than brand names when writing prescriptions. It has been demonstrated that formularies enhance prescribing and lower expenses. It was the responsibility of the clinical pharmacy service to make sure that prescribing followed these formulary recommendations. After several years of overspending on drugs, the implementation of the Formulary strategy led to an underspend. A London Teaching hospital used a limited medications list, and Baker and others described a similar experience. They discovered that there was a consistent decrease in drug spending from 1968 to 1975, which they attributed to the implementation of a policy on the use of medications.
The policy’s utilisation of clinical pharmacists to track adherence to the chosen medication list was a critical component. This procedure included ongoing conversations between prescribers and pharmacists who urged prescribers to conduct self-audit and peer reviews. The implementation of a restricted drug policy was also discovered to be a successful method of preventing the use of novel substances. In the 1980s, the majority of significant hospitals released formularies. Several issues with the formulary process’ implementation were discovered in a 1986 report on the implementation of hospital formularies. These included a lack of adaptability, few updates, and insufficient communication to prescribers regarding drug use.
The pharmacy profession decided to endorse the formulary approach, and clinical pharmacists who were helped by Drug Information pharmacists have utilised them as a training tool for junior doctors. The introduction of information systems that provide details of drug use by prescribers within the hospital has helped with the audit of the impact of formularies. A lengthy study published by Feely illustrated the necessity of ongoing reinforcement of the formulary message by an active sales team, clinical pharmacists. Two hospitals in Ireland were the sites of this investigation, clinical pharmacologists and pharmacists in one hospital actively marketed and promoted the introduction of a hospital formulary. Without any active promotion, a comparable formulary was used in a second hospital. The effect of the formularies on drug expenditures and the standard of prescribing in the two hospitals were studied prospectively. Feedback on prescribing practise, peer comparisons, and drug information were the interventions employed in the hospital with active promotion. During the intervention period, prescriptions for generic medications rose, while the improper usage of third- generation cephalosporins dropped. Drug expenses rose over the same period in the comparator hospital with the same formulary but no interventions. The changes in prescribing were not maintained and drug expenditures rose during the study’s third year, which saw no interventions in either institution. The findings highlight the necessity of continuing to reinforce the promotional messages required to establish effective prescribing practices, with pharmacists working as the “in-house” sales force in direct rivalry with the pharmaceutical sector.

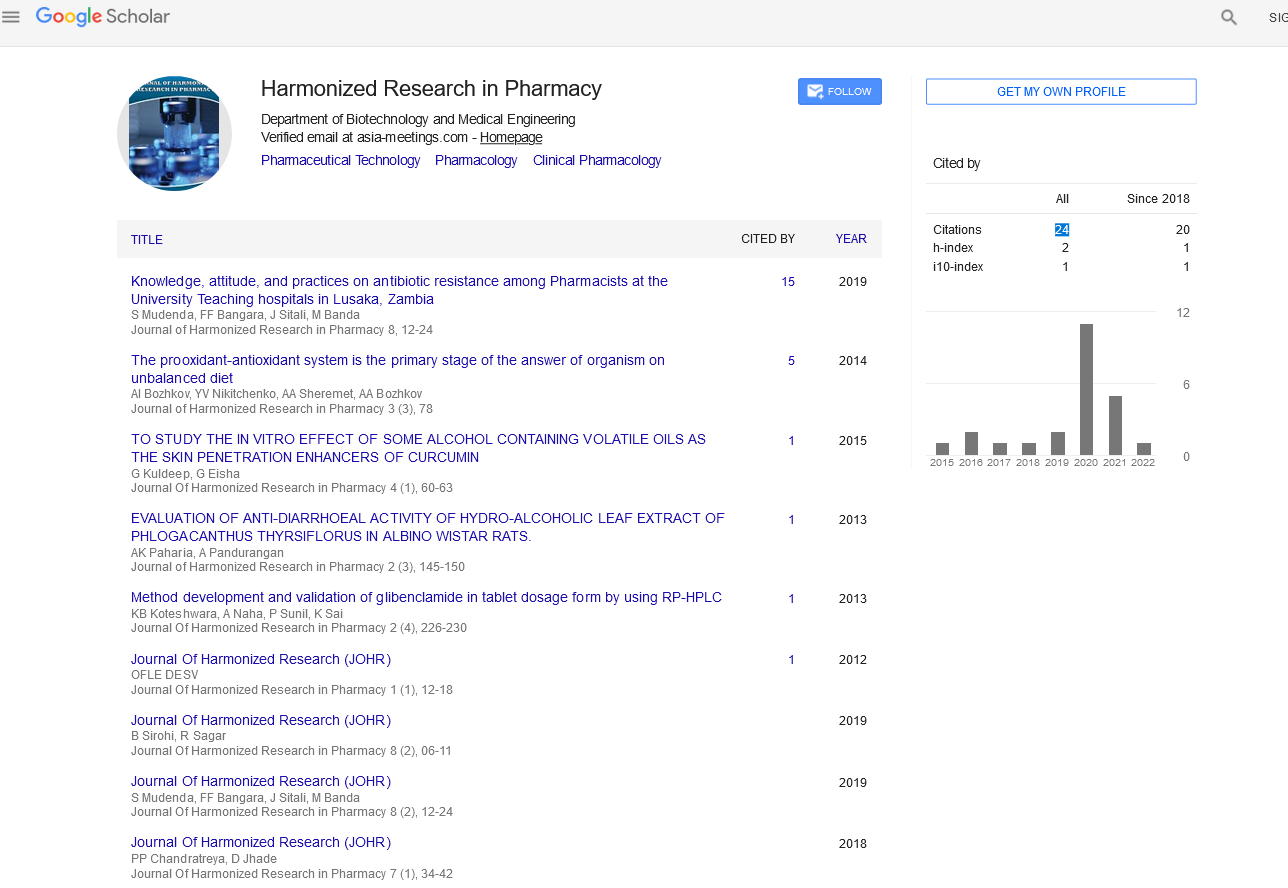
Google Scholar citation report
Citations : 147
Journal of Harmonized Research in Pharmacy received 147 citations as per google scholar report