Commentary - (2022) Volume 11, Issue 2
DRUG DELIVERY FORMULATIONS BASED ON LIPIDS DEGRADATION DURING NEBULIZATION
Darwita Mima*Received: May 27, 2022, Manuscript No. JHRP-22-69507 ; Editor assigned: May 30, 2022, Pre QC No. JHRP-22-69507 (PQ); Reviewed: Jun 13, 2022, QC No. JHRP-22-69507 ; Revised: Jun 20, 2022, Manuscript No. JHRP-22-69507 (R); Published: Jul 30, 2022, DOI: 10.30876/2321-0958.22.11.184
Description
For active medicinal substances that are intended to be administered in a way that specifically targets the lung area, nebulization has several advantages over alternative delivery methods. As the drug is given directly to the desired site of action in the lung, the intended therapeutic effect can be initiated in the affected area more quickly, painful intravenous injections can be avoided, and less medication is needed overall. Compared to oral or intravenous administration, this route of delivery often produces less systemic side effects. Liposomes or lipid nanoparticles can be used to encapsulate drugs to further reduce side effects. In fact, encapsulating medications in traditional liposomes has a number of demonstrated benefits, including targeted drug delivery to particular tissues and protection against drug degradation. Such protection is attractive to vaccine and medicine producers, for instance in the case of RNA drugs that are susceptible to RNase degradation. Additionally, the usage of LNPs makes the drug’s cellular absorption easier and more effective. LNPs are a new generation of liposomes that are designed specifically for the effective distribution of diverse active medicinal components. They differ from liposomes in that they have less internal water content. However, the lipid-based nanoparticle drug formulations may suffer damage due to shear degradation during the nebulization process, which results in the loss of the originally entrapped active medicinal components, especially in the case of hydrophilic materials. This is a result of the nanoparticles breaking due to a high shear stress.
In order to minimize the damaging effects of shear stress on nanoparticle stability and maximize the rate of deposition and effectiveness of the formulation in the “deep lung,” the development of lipid-based nanoparticle carriers for inhalation is therefore concentrated on strengthening and rigidifying the nanoparticles. The recently FDA-approved nebullizable liposome formulation of the antibiotic Amikacin serves as an illustration of a successful lipid-based nanoparticle drug formulation. Its success is attributed to the joint development of a shear-stress resistant nanoparticle formulation of cholesterol-enriched Dipalmitoyl- Phosphatidylcholine (DPPC-CH) with a liposome size of around 300 nm and a PARI eFlow vibrating mesh. There are several clinical benefits to encapsulating medications in protective lipid- based nanoparticles and nebulizing them into the target location of the body. Nebulization, however, has the potential to destroy delicate nanoparticle structures, such liposomes, leading to the loss of pharmaceutically active components. There are two different lung inhalation devices: Continuous jet nebulizers with- out an actuator and high-frequency piezo-actuated vibrating mesh nebulizers. The three different types of liposomes-DPPC, DPPC- CH 50:50, and DPPC-DSPEPEG2K 100:1-each contain calcein as a model for a negatively charged medication in their inner aqueous compartment in order to guarantee that the findings are applicable to other lipid formulations. Calcein is a self-quenching substance that can be used to test for membrane leakage. The maximum fluorescence intensity, Fmax, that was produced when the liposome membrane was destroyed by the surfactant TritonX100 allowed for the quantification of the relative fraction of drug released prior to complete membrane disruption, X (in percent), by dividing the fluorescence intensity F (before or after nebulization) by Fmax. The energies required for nebulization are substantially higher, vibrating mesh nebulizers cause model liposomes to release more than 10 times as much encapsulated material as continuous jet nebulizers. This finding emphasises the significance of using a mild nebulization technique when lungs are administered shear-sensitive medication formulations, such as those based on lipid nanoparticles.

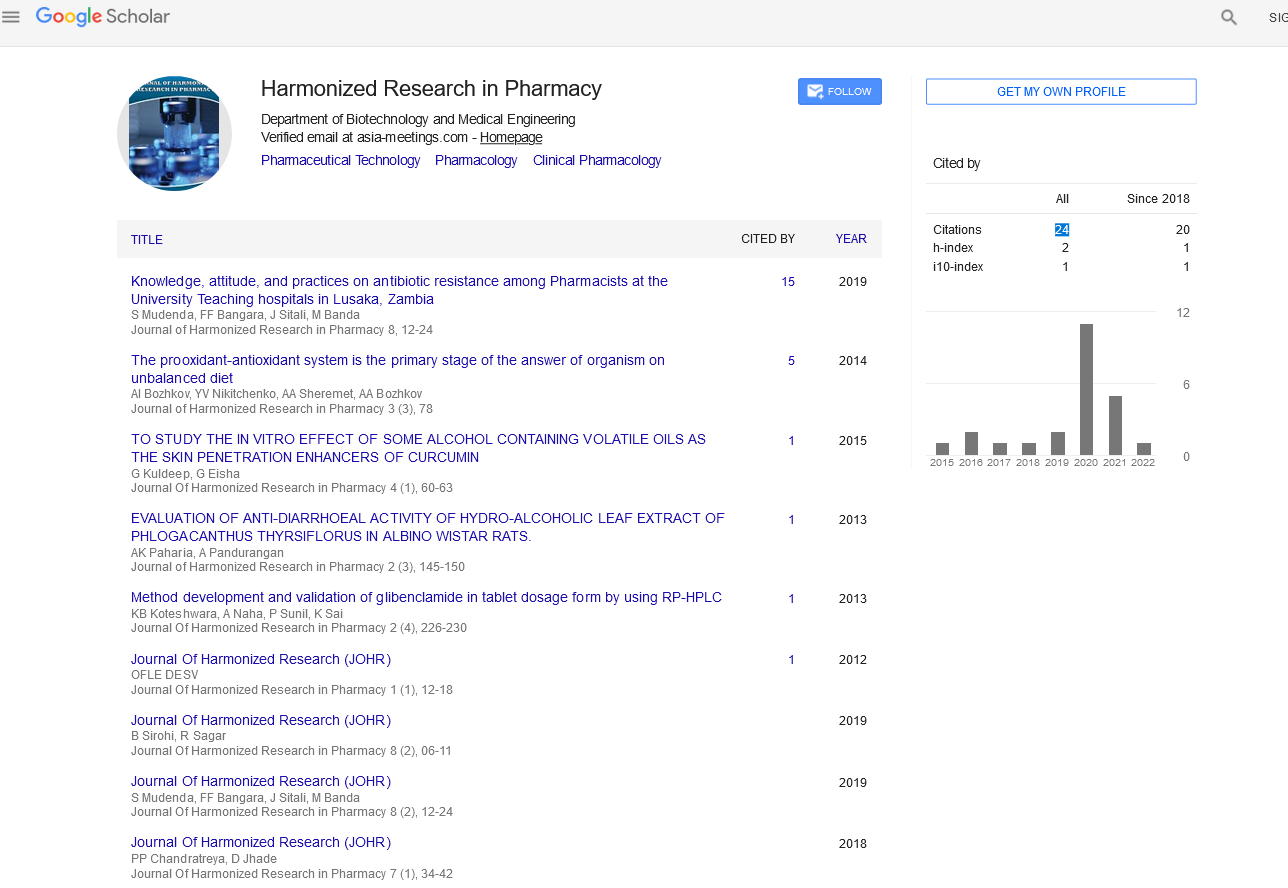
Google Scholar citation report
Citations : 147
Journal of Harmonized Research in Pharmacy received 147 citations as per google scholar report