Commentary - (2022) Volume 11, Issue 3
FACTORS ASSOCIATED WITH ADHERENCE TO PHARMACOLOGICAL AND NON-PHARMACOLOGICAL TREATMENTS IN PATIENTS WITH BORDERLINE PERSONALITY DISORDER
Ahmad Wouden*Received: Sep 01, 2022, Manuscript No. JHRP-22-77682 ; Editor assigned: Sep 05, 2022, Pre QC No. JHRP-22-77682 (PQ); Reviewed: Sep 19, 2022, QC No. JHRP-22-77682 ; Revised: Sep 27, 2022, Manuscript No. JHRP-22-77682 (R); Published: Oct 05, 2022, DOI: 10.30876/2321-0958.22.11.185
Description
An extreme degree of instability in impulsive sentiments, identities, relationships, and behaviours is a hallmark of Borderline Personality Disorder (BPD). Due to aberrant prefrontal brain activity during stimulus processing, patients with BPD are hypersensitive to emotional cues. The frequency of BPD, a serious mental disease, is between one and three percent in the general population. The development and control of impulses as well as a person’s experience of life were determined by the ongoing change in the unpredictability of relationships. It is estimated that 84% of BPD patients exhibit suicidal behaviours, and 8% of them die by suicide. BPD is a serious condition that accounts for 20% to 40% of psychiatric admissions. For both the patient and the community, BPD results in numerous issues. The repeated and severe harm brought on by this disorder affects a person’s entire life, including their employment, their likelihood of dropping out of school, their relationships with friends, family, and co-workers, as well as their ability to get married and maintain stable and high- risk sex relationships. Nearly 11% to 69% of patients take drugs, 22% of these patients are alcoholics, and 25% to 50% of female convicts have BPD. Adherence is a complicated behaviour that can be impacted by a number of variables, ranging from small treatment refusals to inappropriate use of medical services or even therapy desertion. These variables frequently vary on the patient. Fear of developing a medicine dependency is the most prevalent irrational fear that is linked to rejection. Numerous researches on patients with personality disorders, schizophrenia, and bipolar illness have shown that one of the key concerns in treatment is the patients’ acceptance of the treatment. It appears crucial to assess medication and non-medication adherence in these patients given the prevalence of BPD, the requirement for long-term pharmacological and non-pharmacological therapy, the high cost of care placed on the healthcare system, and the absence of studies in Iran. It is hoped that by addressing modifiable factors, patient adherence will increase, leading to an improvement in function and a decrease in symptom recurrence and readmission.
This study sought to identify the variables influencing the adherence to both pharmaceutical and non-pharmacological treatment in 94 BPD patients who were sent to the outpatient clinic of the Tehran Psychiatric Institute. The findings of this study revealed that individuals with good, poor, and relative medication adherence did not differ significantly in terms of gender, occupation, education, marital status, history of psychiatric hospitalisation, history of self-harm and suicide attempt, and history of substance use. However, individuals with good, poor, and relative adherence to psychotherapy had considerably diverse educational backgrounds and hospitalisation histories. The research also revealed no statistically significant differences in terms of gender, occupation, education, marital status, prior mental hospitalizations, prior self- harm and suicide attempts, and prior drug usage and compliance.
The results of our study demonstrated that poor adherence was most frequently caused by a better attitude toward psychotherapy, a negative attitude toward medication, and a fear of pharmaceutical dependence. In order to assess the pharmacological treatment, medication, and psychotherapy adherence in BPD patients. In this study, people with varying levels of psychotherapy compliance were found to have discontinuation of treatment due to dissatisfaction with the doctor, lower education, a history of psychiatric hospitalisation, and discontinuation of treatment due to the high expense of psychotherapy. However, there was no significant difference between those who adhered to various medications and forms of psychotherapy and those who did not, when taking into account other factors like gender, occupation, education, marital status, history of psychiatric hospitalisation, history of self-injury, and history of substance use; All of these findings were consistent with our research. In our investigation, patient adherence was generally unaffected by demographic characteristics, histories of self-harm and suicide, histories of substance use, or comorbidities.

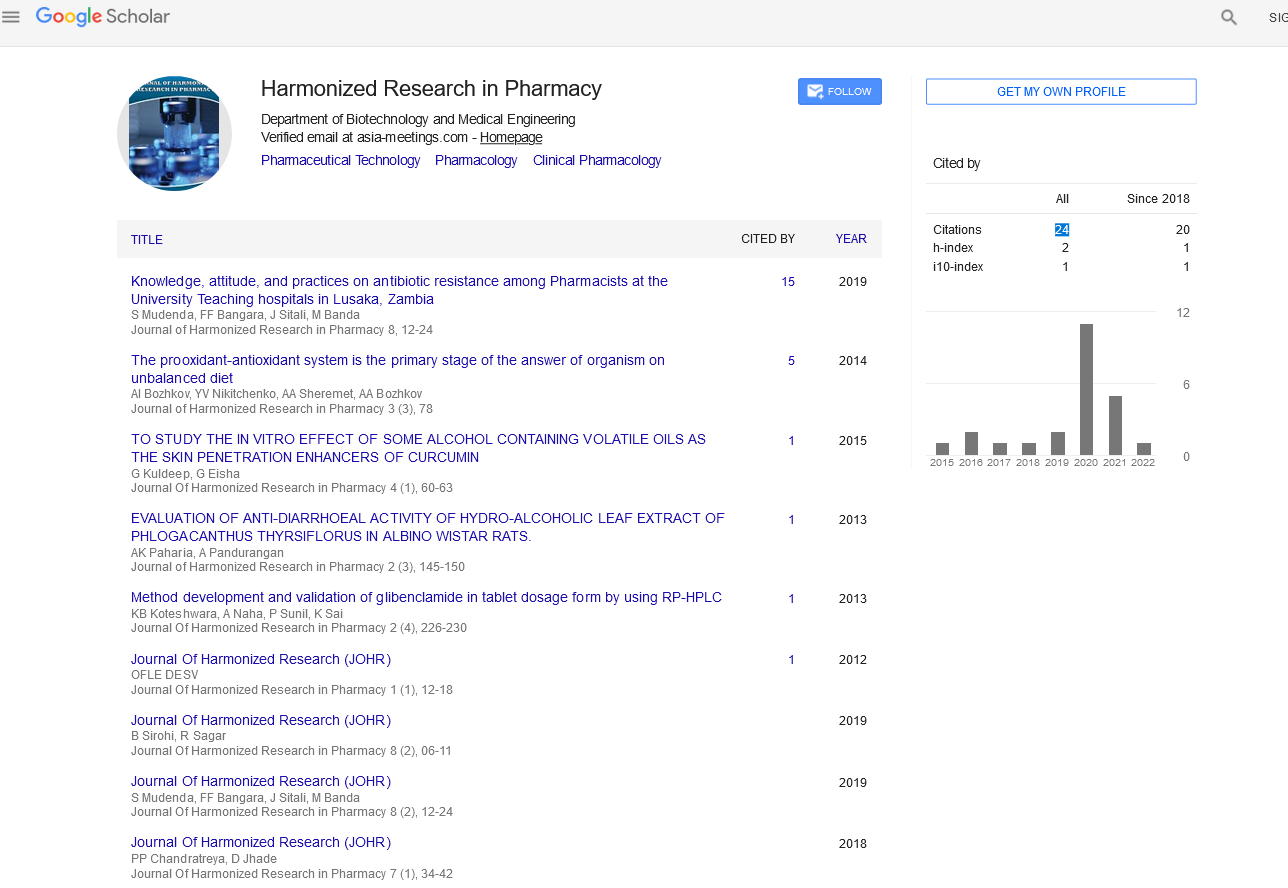
Google Scholar citation report
Citations : 147
Journal of Harmonized Research in Pharmacy received 147 citations as per google scholar report