Commentary Article - (2021) Volume 10, Issue 2
NOVEL INDICATORS OF DRUG INDUCED KIDNEY DAMAGE IN RENAL TRANSPLANT
Liu James*Received: Dec 06, 2021
Description
Kidney damage that occurs in many diseases is poorly recognized due to the lack of early markers and is predominantly recognized in severe renal lesions with renal dysfunction. Urine or blood BM helps diagnose early kidney damage and provide early intervention. In nephrology, the most commonly used BMs are serum creatinine and Blood Urea Nitrogen (BUN) and proteinuria, or blood cells in the urine. However, these parameters are insensitive, cause delays in diagnosis and / or treatment, and are less specific, so renal biopsy should be used to properly characterize the injury. Unfortunately, renal biopsy is an invasive procedure that exposes patients to rare but life-threatening hemorrhagic adverse events. During the last decade, efforts have been made to discover and characterize new early diagnostic urinary.
Simultaneously, the FDA and EMA have also encouraged research programs to identify and qualify early BM of drug induced kidney injury. These new renal BM can be classified as functional BM or tissue injury BM. Micro albuminuria is a BM of glomerular injury and/or impaired tubular proximal protein reabsorption. Cystatin C is a lowmolecular weight protein freely filtered in the glomerulus and then reabsorbed by renal proximal tubules. In addition to its potential role as a biomarker for blood glomerular filtration rate, urinary cystatin C is a marker of proximal tubular dysfunction. Retinol-binding protein 4, a protein in the lipocalin family, is a BM for proximal tubular reabsorption disorders. Nefrin and podocin (a component of the podocyte filtration division), Killer 1 (a protein that interacts with the C-terminus of podocytes), and podocalyxin (a major component of the podocyte sugar coating) are new BMs for glomerular injury. N-Acetyl βD Glucosaminidase (NAG) (proximal tubule cell brush margin enzyme), neutrophil zeratinase- associated Lipocalin (expressed at low levels in neutrophils and various tissues, but induced in epithelial cells during inflammation Proteins), Kidney Injury Molecule 1 (KIM1), a transmembrane protein whose expression is increased in the case of proximal tubular injury and / or regeneration) and crusterin (a protein associated with cell debris and apoptosis clearance) are proximal. Among these proximal tubular cell biomarkers, NGAL is expressed at low levels under normal conditions, but is rapidly upregulated after renal injury, resulting in sensitive monitoring of DIKI in clinical trials. It is a very attractive biomarker for you to do. Osteopontin, a secreted glycoprotein, and calbindin, a calcium-binding protein in the kidney, are used as markers for distal tubular damage. Aquaporin 2 promotes water absorption, and its elevated urinary levels are a marker of collecting duct damage. Monocytic Chemotactic Protein 1 (MCP1) is an inflammatory marker that mobilizes leukocytes to the site of inflammation. Most of these new renal BMs are still being studied in humans and while NGAL appears to be the most promising, it has not been validated as a clinically useful BM in daily work. The association between histological lesions, the current gold standard of nephrology, and blood or urinary levels of these new BMs has not yet been established in clinical practice. In renal graft recipients, renal biopsies are performed as a routine evaluation mainly in the first semester after transplantation. Renal dysfunction is frequent after transplantation and may be linked to drug toxicity, immunologic injury of humoral or cellular origin, infectious injury, or recurrence of the initial disease for which no current BM are available to discriminate the type and the consequence of injury. Therefore, biopsies are routinely performed to identify initial lesions. These graft biopsies performed in every graft recipient represent an ideal opportunity to evaluate new renal BM and assess their association with renal histopathology, the current nephrologic gold standard.
Conclusion
The newly studied BM did not appear to perform better than traditional BMs in type or identification.. However, NGAL may improve slightly. When hesitating in the early stages of a kidney transplant Tubular necrosis may help distinguish between ATN recovery and acute transplant rejection. This is a common situation in clinical practice and early detection is really necessary. A non-invasive diagnostic tool to potentially avoid some graft biopsies and reduce diagnostic delays. In this situation, future prospective studies may focus on new BMs like NGAL and improve their use.

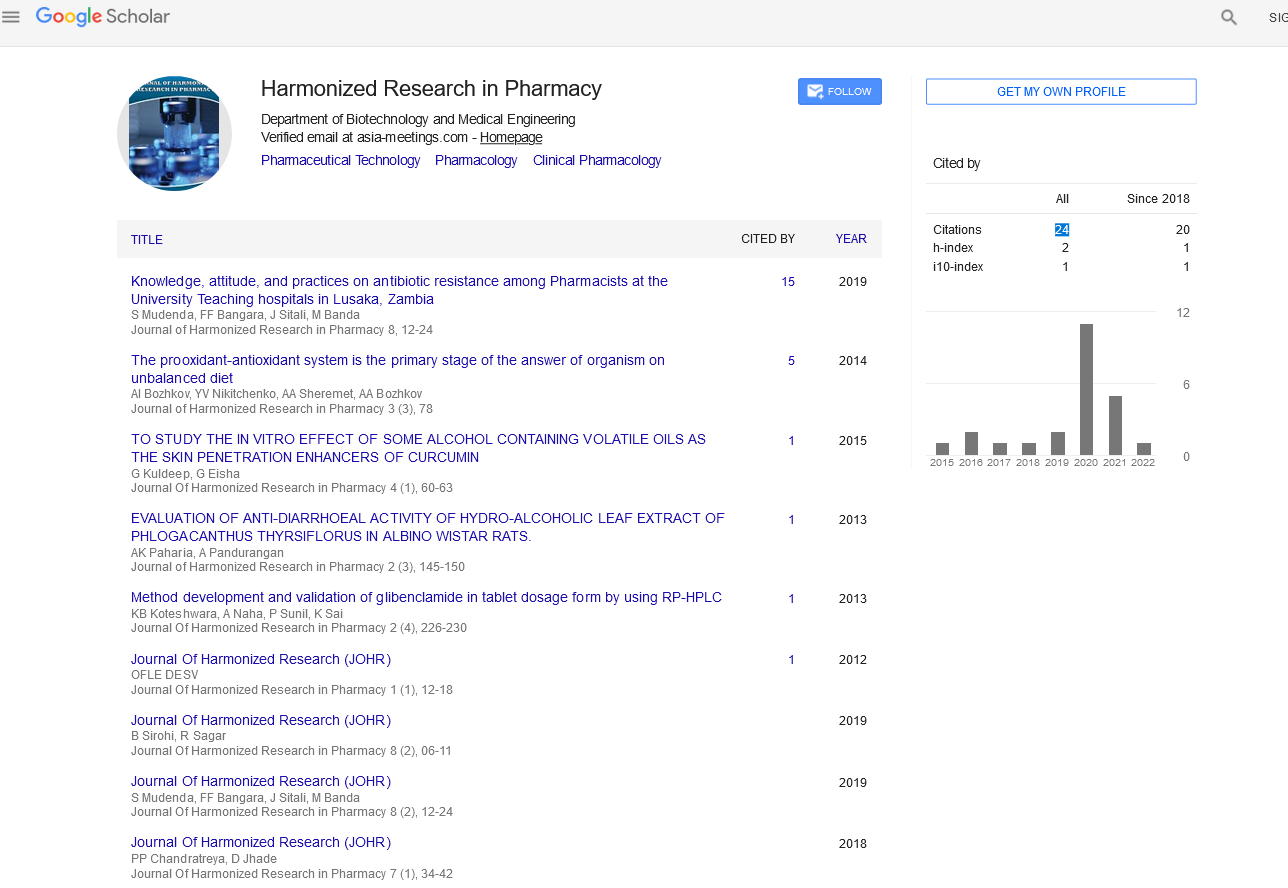
Google Scholar citation report
Citations : 147
Journal of Harmonized Research in Pharmacy received 147 citations as per google scholar report